Appendix 1: Childhood vision screening after the neonatal period – procedure
Choice of test
The gold standard test for adult VA testing is generally considered to be a logarithmic Landolt C test. Any VA test used for screening should approach this gold standard as closely as possible. The Landolt C test is, however, difficult for use with children. Most adult clinical charts use letters, which have been chosen to be of similar visual difficulty and based on the Bailey-Lovie principles1.
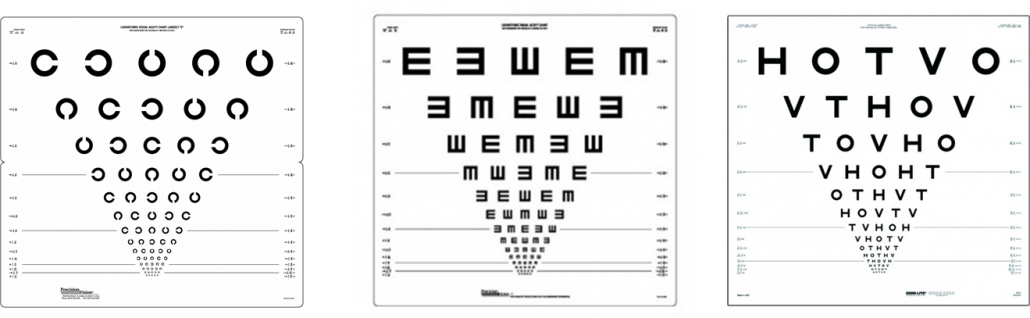
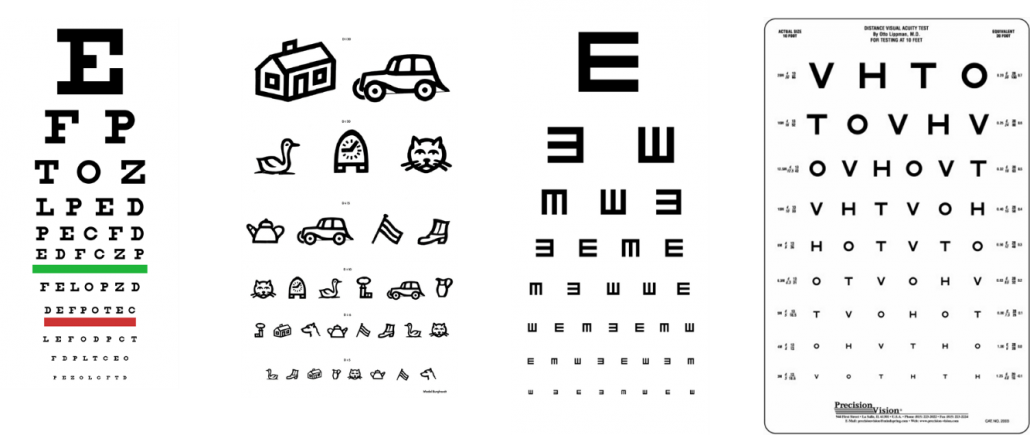
We do not recommend any specific test charts, but it is important that any test has published validated age norms2 and adheres as closely as possible in terms of logarithmic space-to-optotype ratio, as in the Bailey-Lovie chart3, recommended by the ICO in 1984 or according to the European ISO 8596 Standard (EN ISO 8596:2017). The European Standard for Vision Measurement states a VA chart should contain at least 10 lines of optotypes. Many charts with a logarithmic progression maintain a consistent ratio between optotypes and spacing of letters and lines, proportional to the optotype size (see FIigure 1). Visual acuity measured with these logarithmic progression charts can be recorded in logMAR, fractional or decimal notation (see notation section below) Decimal progression and Snellen charts do not have the same proportional difference between lines at different points on the chart (see Table 1 and Figure 4) and are being phased out of the scientific literature, orthoptics and ophthalmology. Charts with a decimal linear scaling from 0.1 (low visual acuity), 0.2, 0.3 etc. up to 1.0 (good visual acuity) are not appropriate because they do not follow a logarithmic progression and could lead to wrong decisions about failing the test and referral. They should be avoided clinically, although in many countries this change has not been widely adopted.
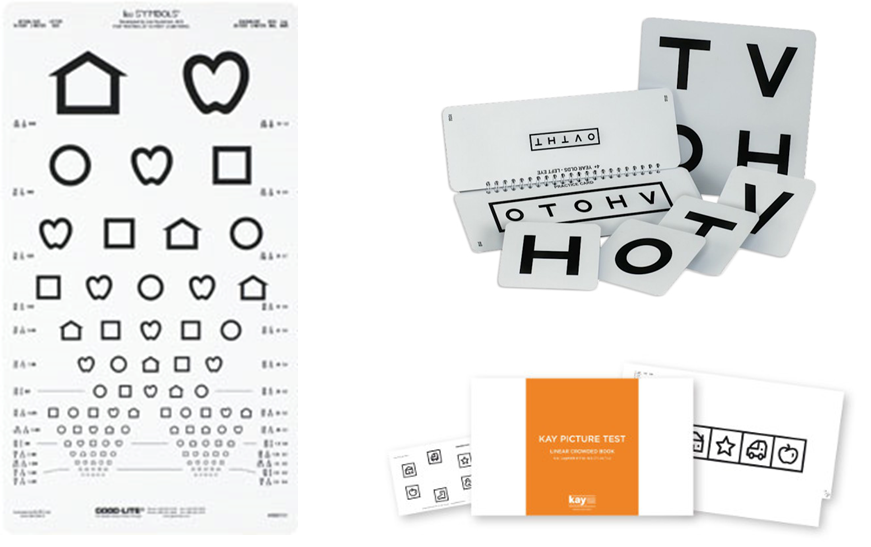
Tests designed for pre-literate children can use the Tumbling E format, letters or symbols which can be used with matching cards. Some use a flip booklet format with a single row of letters surrounded by crowding bars e.g. Keeler logarithmic crowded test, so that young children do not get confused by too many letters on the chart. The ‘Tumbling E’ is somewhat easier for young children, although somewhat less in quality than the Landolt C. Some symbol tests such as the LEA symbols and Kay Pictures are calibrated against the gold standard adult tests (Landolt C) and thus also a possible choice. In countries with early school entry age, young children may be familiar with letters, so letter charts may be feasible for these children (crowded logarithmic tests). Most children will be able to use a matching card even if they cannot name letters or symbols. Single letter tests should be avoided as they compare very poorly to linear logarithmic tests particularly in amblyopia. Picture charts such as the Amsterdam Picture Chart, do not compare well to logarithmic charts, are not well validated, and may contain pictures that modern children may not recognise e.g. old fashioned cars, so should not be used4. Some pictures may also be culturally specific and disadvantage children from other ethnic backgrounds.
Many digital screening options use laptops or tablet devices to present a letter chart. The best have been well calibrated as above so are an alternative option. Small screen size on portable equipment can be a limitation, necessitating making testing distance closer than physical charts need to be. The closer the testing distance, the more critical it is that children do not move closer to look intently at small letters. Whatever test is chosen it is important that it has been validated, uses a linear optotype format adhering as closely to the gold standard tests above and has published visual acuity norms and confidence limits for different age children. A definition of what is abnormal VA must be based on the confidence limits for normal vision for the age of child and the test.
Figure 1: illustrates acceptable tests using the logarithmic format
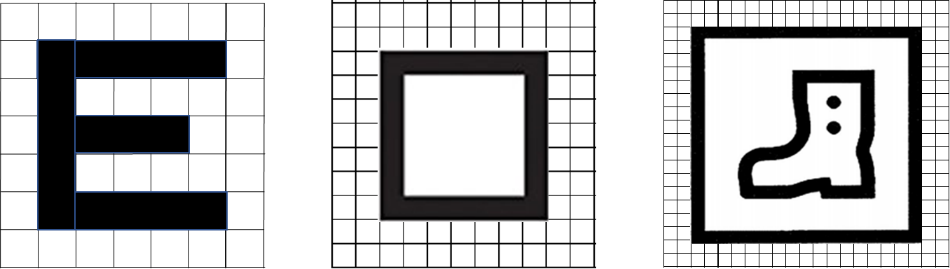
If picture tests are used for children who cannot do a letter test e.g. LEA symbols or Kay Pictures, it is important to understand that the symbol construction differs from the construction of adult tests, in that the proportions of line thickness to space is different. E.g. Lea symbols are drawn from a 7×7 grid and Kay Pictures from a 10×10 grid (Figure 2). They may be well calibrated against gold standard tests, but even if validated, they may differ from other or adult tests (for example the Kay Picture test tends to return slightly better acuities than the LEA or Landolt C, so referral thresholds might need to be different5.
Figure 2: construction of Snellen symbol, LEA test symbol and Kay Pictures symbol
Test distance may be between 3 and 5 metres and some tests are calibrated for more than one distance, but most specify a single distance. In younger children the closer test distance may improve cooperation, but the closer the testing distance, the more important that it is adhered to exactly.
Figure 3: child vision tests based on logarithmic principles (LEA, HOTV and Kay Pictures)
Figure 4: types of non-logarithmic charts using Snellen optotypes, pictures and decimal progression of optotype size which are not recommended
Charts illustrated in Figure 4 are not advised because they do not adhere to any or all of the Bailey-Lovie logarithmic principles in terms of symbol construction, equality of recognisability, line or character spacing.
Checklist when deciding on which test:
- Is it a logarithmic chart?
- Is it as close to a gold standard test as possible?
- Has it been validated against a gold standard test with published age-related norms?
In practice, it makes sense to decide on a first line choice of optotype (e.g. letters or E tests), but to also have an alternative optotype (e.g. LEA symbols) which can be used if a child does not cooperate with the first line optotype if a re-test would be difficult to rearrange e.g. in remote rural areas.
It is, however, critical to understand that inaccuracy of screening is more likely to be due to the tester, not the test. So even if automated methods are adopted, children still need supervision to ensure attention, motivation and co-operation and to prevent attempts to peek around an occluder.
Visual crowding
In amblyopia the recognition of optotypes in a line of letters or a word is more difficult than for a single letter (‘the crowding effect’) and letters at the beginning and ends of lines may be more recognisable. Very close spacing of optotypes may hamper cooperation in young children due to physiological crowding.
Crowding is a normal phenomenon, but it is greatly exaggerated in amblyopia, therefore presenting one single optotype or few optotypes with large spaces between them may lead to underestimation or missing of amblyopia. According to ISO 8596:2017 each line must have at least 5 optotypes. Crowding can also be standardised by adding a high contrast frame around the optotypes (e.g. the Keeler crowded logarithmic test flip booklet, which only presents one size of letters at a time).
Notation
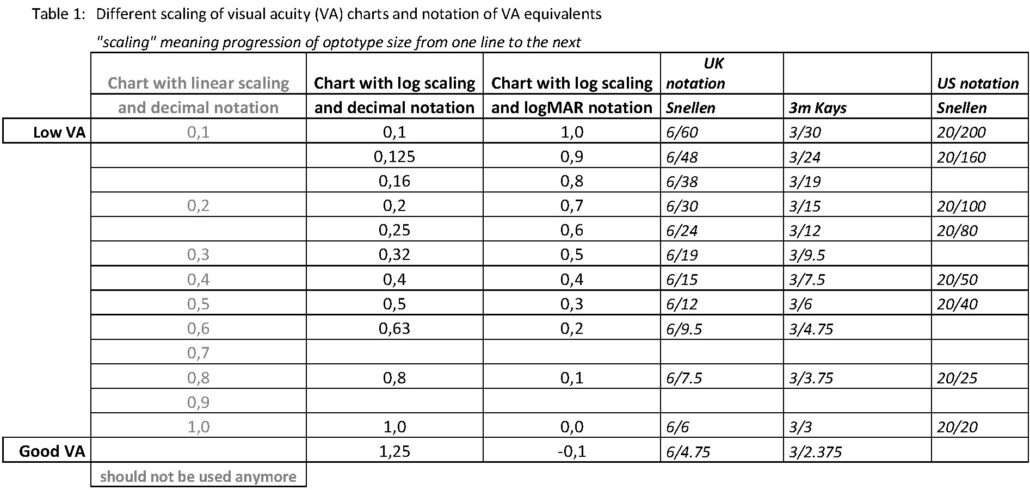
Mean ‘normal’ visual acuity in an adult is visual acuity 1.0 = 0.0 logMAR being 1′ arc angular visual resolution equal to the size of the gap in a 5′ Landolt-C optotype with 3 out of 5 guessed correctly. Visual acuity can be expressed in many different ways and conventions often vary between countries. Snellen notation expresses letter size as a fraction of testing distance, with good vision being e.g. 6/6 (metric e.g. UK) or 20/20 (feet e.g. US) or its decimal (e.g. 1.0, as used in much of Europe). LogMAR notation results in 0.0 meaning good vision and 1.0 poor, while in decimal notation 1.0 is good and values near 0.0 are poor (see Table 1).
Table 1 also shows that, for example, the difference between decimal VAs of 0.1 and 0.2 is much larger in logMAR terms than between decimal 0.4 and 0.5. VA charts with linear scaling of decimal values 0.1 are not appropriate because they do not follow a logarithmic progression, and could lead to wrong decisions about failing the test and referral.
This can very easily lead to confusion, especially if logMAR notation is used by screeners in a country where decimal notation is the norm and clinicians still use decimal notation. Modern visual acuity charts often show several notations for the same line, and it is important to read the correct one (details about different visual acuity notation on visual acuity charts are shown in the Table 1 below).
LogMAR is the internationally recognised standard . Great care must be taken in training, recording and communication so confusion does not arise. It is important that the screening records always show which optotypes were used, which spacing between them and which type the visual acuity notation is.
Table 1: different scaling of visual acuity (VA) charts and notation of VA equivalents
It may be helpful to provide in the screening forms all visual acuity levels shown by the respective chart for the right and left eye separately, so that the obtained values can be circled or underlined – or clicked in case of electronic records.
There is an international consensus that logMAR notation is the gold standard, but in many countries decimal or Snellen notations are still the norm in clinical practice. To avoid confusion, for referral after failed screening it makes sense to use the notation known to the ophthalmologists in that country, and possibly logMAR notation additionally (clearly specifying which value is which notation). Training of screeners and those auditing any reported outcomes must ensure the correct notation is used.
Pass/referral criteria
The criterion for passing or failing a visual acuity screening test has to be specified. It depends on the children’s age and the visual acuity chart used (especially the spacing of the optotypes within a line, or the ‘crowding’) and needs to be related to normative data for the particular test used and age of the children. Normal ranges in children typically show slightly lower acuity and wider confidence limits.
ISO 8596:2017 states that to pass a line three out of five letters on the line must be identified correctly . This is scientifically valid in tests like the Landolt C or tumbling E because a test with 4 possibilities best measures (highest specificity) at 62.5%, because it is halfway between 100% good at large E’s and 25% good at small E’s. Thus a child seeing 3, 4 or 5 letters on the 0.2 line would pass the test and be recorded as having a VA of 0.2.
According to some literature[/fusion_builder_column]
Services must decide whether to repeat screen or refer children on the referral borderline or those who were too immature to understand the test. A ‘repeat before referral’ policy saves expensive false referrals and may only mean a few weeks delay for the few genuine cases. These criteria should be revisited during regular evaluation. This is particularly important when testing the youngest children who may ‘fail’ due to loss of concentration (especially of the second eye tested).
If a child does not reach the ‘pass’ criterion and the screener decides that cooperation was good, the child may be referred for ophthalmological assessment. If the screener decides that the failure was possibly due to lack of cooperation or fatigue, retesting may be done with the same optotypes or with a second line of optotypes on another occasion, starting with the other eye if necessary. If understanding the task is the problem, an easier test e.g. LEA symbols, could be tried. This could be later in the same day, or on a subsequent visit within a specified period. Experienced testers are much more accurate than novice screeners, and skill and confidence are helped by regular audit and feedback from outcomes.
Additional orthoptic tests
Many screening services in Europe use additional orthoptic tests, such as cover tests, motility assessment, binocular vision or stereo tests. Many of these tests require a high level of skill. Small defects are easy to miss so sensitivity and specificity are low, especially if not carried out by trained orthoptists. Larger defects usually present to ophthalmology services before screening anyway due to parental concern.
Evidence of additional cost-effectiveness of adding these tests in improving the detection of amblyopia is limited. In 2013 the UK recommended a single visual acuity screen without additional orthoptic tests.
Decision makers need to agree on referral criteria if cost-effectiveness of an amblyopia screening service is to be maintained. For example, are asymptomatic children with non-amblyopic small angle or intermittent strabismus, reduced stereopsis or convergence insufficiency a target for the screening, or is the service concentrating on low vision and amblyopia. Small changes to referral criteria or adding/removing a test may make significant differences to referral rates and costs.
Countries may make different decisions. Some countries (often those with high incomes) have a high acceptance of screening and easy access to medical care. Referral of mild, or non-sight-threatening defects such as intermittent exotropia or slightly defective binocular vision might be acceptable and affordable for parents. Other countries have poorer public health awareness, few paediatric ophthalmology services, and accessing them could be a huge financial burden to very low-income parents. Here, a decision might be made to only screen for the most severe problems. Detecting mild problems which do not impact on a child’s education or future employment prospects may be an unaffordable luxury. One of the reasons that amblyopia fulfils the WHO criteria as a screenable condition is that untreated unilateral amblyopia can lead to blindness and a large burden on families and society if the better eye is lost in later life, and especially old age. This is not the case for conditions such as strabismus, mild myopia or weak binocular vision.
Preparation for the testing
Administrators or screeners should establish visit dates with the school, clinic or kindergarten and confirm room bookings and lists of children to be tested. Decide how children who are absent on the test day will be tested within the screening timescale.
If not embedded in the community, the screener should establish rapport with local staff and make sure they know what will happen, so they can explain to children and parents and reinforce support for the screening.
Ask staff to tell the screener about any child who might need specific handling (shy, hyperactive, special needs, non-native language speaker). Establish what provision will be made for children with special needs or disabilities. Some countries mandate that all such children are tested more fully, but in other countries these children may not even be in school. There may be national guidelines mandating more detailed assessment of children with some disabilities or genetic conditions.
Inform parents (and if applicable preschool or school teachers) about the planned screening and get informed parental consent or refusal (see chapter 4e).
Depending on the location, parents or teachers may prepare the children for testing. Images of the test symbols used (for example LEA or Tumbling E’s) may be put in the envelope of the letter inviting the parents for the screening so that they can practice with their child beforehand at home. This reduces the number of failed measurements.
Prepare a quiet and secure room, large enough (depending on the test distance for the visual acuity chart used) for assessments, with the possibility to present the visual acuity chart at eye height of the children. The European Standard for Visual Acuity Measurement ISO 8596 recommends that the chart’s luminance (‘brightness’) should be between 80 and 320 cd/m2. Basically, the charts should be well and adequately illuminated in a normal daylight conditions medical examination room (the examination room of an ophthalmologist is usually darker). The chart should not be illuminated with extra light spots. Avoid direct sunlight or shadows on the chart. The luminance of the visual acuity chart can be measured using a luminance meter if necessary.
An appropriate space for testing should:
- be quiet and free of distractions
- be close to where the children will be collected from
- have good lighting
- have suitable chairs
Suggested equipment required in screening sessions:
- visual acuity test(s)
- key card(s)
- device for covering the non-tested eye (tape or occlusive glasses)
- list of children to be screened
- confirmation of parental consent or refusal, depending on whether an opt-in or opt-out consent policy is used (see chapter 4e)
- recording method (paper or digital)
The distance from the child’s eyes to the visual acuity chart can be marked with a mark on the floor.
The screener should receive a list of children to be screened, with information about children with special needs or comprehension problems who might need help or more specialist testing.
If the testing area is not close to the children, for example across a playground or upstairs, availability of a helper (classroom assistant/parent/older responsible child) is very useful to fetch the children to make most efficient use of the screener’s time.
Procedure of visual acuity assessment in children
Start by confirming identity and consent, and that the child understands the screener. If a child already has glasses they should be worn during the assessment.
The child may sit on a parent’s lap, but may also sit or stand alone. The child should not lean forward excessively or sit on the tip of the chair. Ideally, if practically and financially feasible, two people should be present to screen children aged 4–5 years: the screener to undertake the test and the other person to sit by the child to offer encouragement, confirm results on the key card if used, and to supervise the child, to ensure the child does not lean forward, keeps head straight, and does not peep. This helper could be a classroom assistant, volunteer parent or even a responsible older child.
Explain to the child in comprehensible terms what is expected of him. Practice the measurement first binocularly at a short distance, for example 40 cm, to ensure the child understands the task, then begin the actual test monocularly. If they do not understand, move onto an easier test such as a validated picture test, and record clearly that that was done. If a re-test would be possible, a later attempt at the same test may be preferable than a less accurate result from an easier test.
Always start with the same eye (right eye), unless it is a repeat examination, then start with the ‘suspected’ eye.
Provide a method for secure covering of the non-tested eye, for example two pairs of occluded glasses frames of different colour, where the right or the left eye is covered so that peeping is not possible. Sticky eye patches prevent peeping more reliably, but many children dislike wearing them so cooperation may be lost.
Never use the child’s or the parent’s hand for covering the fellow eye as a tiny gap between fingers may allow the occluded eye to still be used and amblyopia or low vision can be missed.
Keep looking at the child and never turn your back at the child. Observe the child carefully before and during testing – abnormal head position, eye alignment, eye movement, opacity of cornea or lens, hanging eyelid (ptosis) may reveal pathologies.
Point from below at the optotypes with a finger or a black pen, leaving a similar space to the optotype as lies between the optotypes. Make sure the whole optotype is clearly visible to the child. Encircling the optotype with a pen once is permitted, but do not cover the surrounding optotypes, because in the case of amblyopia, this will provide unrealistically good results and amblyopia may be missed.
Start at the top line. According to ISO 8596 the optotype must be presented no longer than 10 seconds, however young children may need longer to respond. In the case of an incorrect answer, indicate another optotype. If three of the five optotypes are named correctly, go to the next line. Proceed to the last line where three of the five optotypes are named correctly. That is the visual acuity to be recorded. If a child can clearly see the upper lines of a chart, it may be permissible to check fewer larger letters (e.g. one central letter per line) to maintain co-operation for the lines closer to the child’s threshold, when all letters on the line must be tested so the 3/5 criterion can be applied (see section on pass/fail criteria).
The visual acuity value determined should be recorded immediately after testing each eye, using a consistent notation. Recording is sometimes done giving a logMAR value based on each letter seen. All documentation should use the convention of showing the right eye first.
Some children with strabismus, ocular motility defects and abnormal head postures will not have reduced VA. See section on orthoptic tests above.
Encourage the child to guess in case of uncertainty, and use encouraging feedback even if a letter is wrongly identified. Make sure that any accompanying person or (if needed) interpreter does not give hints as to the correct answer.
Make sure that evaluation procedures do not suggest one screener is ‘better’ just because the children they tested were, on average, slightly older.
Useful advice
- Make sure the correct child is being tested. Confirm with someone responsible, because many children will respond to other children’s names or have the same name.
- In large communities where more than one visit is planned per year, it can be best to test the oldest children in the age cohort on one visit and leave the younger ones until the later visit. In small communities, children at both ends of the screening age range will need to be tested on the same visit.
- Decide whether to test a child alone or in a small group (two to four children). If a group is brought into the room together, be very sure that the children not being tested cannot see or memorise the test chart or ‘help’ the child being tested. A shy child will be helped by watching a more confident one perform the test. Time can be saved by teaching the test to the group, rather than individually, but a disruptive, distracted or crying child might distract the others.
- Be prepared to be flexible.
- Make sure that the chosen occluder – patch or occluded glasses cover the eye properly and any attempts to peep can be spotted quickly. A child with an amblyopic eye will think it perfectly normal to try to peep around an occluder or find a peephole near the nose, so a face turn during testing is a warning sign.
- Children with an amblyopic eye may look confused when the good eye is covered up but will rarely say they cannot see.
- If an amblyopic eye is tested first, the child may just appear to be uncooperative. By moving quickly onto the other eye, it is easier to decide if it is general poor cooperation or a genuine vision problem in the eye tested first.
- Get into a habit of testing the same eye first every time (usually the right eye). If the order changes frequently, after 20 children the tester might forget that only one eye was tested. If using occluded glasses, use different colours and always use the same colour first.
- Never say “shall we cover up one eye now?” – an obvious reply is “No”. In an unco-operative child a good strategy is to say “which colour glasses shall we put on first?” The child has then been given some control of the test, but understands that both eyes still get tested. Putting a patch or glasses on a toy might help persuade them to wear a patch. If the child has an obvious strabismus (squint / crossed eyes), or a ptosis (droopy eyelid) that eye is likely to have poorer vision.
- Make sure the children know it is a game, and that nobody will be angry with them if they cannot see a letter. Make sure they are encouraged constantly, for every letter. If they get a letter wrong do not tell them they were wrong. You can say “are you sure?” or “good try – now let’s do another one”.
- Encourage ‘intelligent guessing’. So say “what do you think it might be?”, “have a try, even if you are not sure”. A child who genuinely cannot see a letter will often guess wildly or look away while guessing, while a child at their threshold acuity will keep fixating when having a try. Children do not realise that adults have to make similar guesses during any eye test.
- If a child seems to be struggling at their threshold, say “is it too little to see?” – they often look relieved and say “yes”, when they would not have told you they could not see it if you had not asked.
- Experienced screeners develop a ‘feel’ for a child with a genuine problem compared to one who is just scared or uncooperative. It becomes more obvious with experience, but it really helps if testers get feedback about the referred children, so that they learn from their right and wrong decisions.
- Make sure that parents, teachers, GPs, nurses know where they can go for support and advice once the screener has left. Encourage teachers, GPs and satisfied parents to share their experience of screening and getting treatment for poor vision that they had not expected – especially if there was a good outcome.
- Bailey IL, Lovie JE (1976): New design principles for visual acuity letter charts. Am J Optom Physiol Opt. 53(11):740–745.
- Anstice NS, Thompson B (1997): The measurement of visual acuity in children: an evidence-based update. Clin Exp Optom 97(1):3-11.
- Anstice NS, Thompson B (1997): The measurement of visual acuity in children: an evidence-based update. Clin Exp Optom 97(1):3-11.
- Telleman MAJ, Sloot F, Benjamins J, Simonsz HJ (2019): High rate of failed visual-acuity measurements with the Amsterdam Picture Chart in screening at the age of 36 months. Acta Ophthalmol 97(1):24-28.
- O’Connor AR & Milling A (2020): Normative data for the redesigned Kay Pictures visual acuity test. Journal of American Association for Pediatric Ophthalmology and Strabismus.
- Anstice NS, Thompson B (1997): The measurement of visual acuity in children: an evidence-based update. Clin Exp Optom 97(1):3-11.